 This post is an update and rehash of a previous post due to renewed interest in the topic.
This post is an update and rehash of a previous post due to renewed interest in the topic.
Below is a comprehensive list of forms needed to complete a basic life support, routine inter-facility ambulance transfer in the State of Connecticut in 2015. More medical and billing information and demographics are necessary but in regards to forms that go to the ambulance crew, this it…
None of the information below should be construed as legal advice. If there are questions always consult the proper authority. If you have basic questions on this material please call us or post your question in the comments and we will answer to help the greatest number of interested parties.
Medical Necessity Form (aka Physician’s Certification Statement (PCS) or MNF): An MNF is required on routine, non-emergency ambulance transports where the patient has Medicare as their primary insurance. It is helpful to have on file for beneficiaries of Medicare HMOs as well. The form essentially works as a prescription for ambulance transport. Medicare never pays for wheelchair van transport so this form represents the threshold between wheelchair van (and all other types of transportation) and ambulance. There are some types of transports from skilled nursing facilities (SNF) and hospital where the sending facility is required to pay for the transport and therefore will not issue or sign an MNF.
There is a misnomer that MNFs are not needed on hospital to hospital and STAT transports because they are inter-facility or emergent. They are indeed required regardless of acuity or receiving facility. Although there are some rules around this they are detailed and convoluted. It is best to provide an MNF on every scheduled ambulance transport in which Medicare or Medicare HMOs are the payor.
A Medical Necessity Form alone does not guarantee payment. In fact it does very little in this regard. It must be on file, but the most important factor is the patient’s condition. The patient must be unsafe to travel by any other means. There are more rules regarding repetitive patients in which a new PCS is only needed every 30-60 days.
The rules around the use of an MNF and meeting Medicare’s medical necessity requirements are extensive and cannot be captured adequately here. Aetna and ASM crews are trained, reviewed, remediated and subject to a rigorous quality assurance process in this regard. If you represent a facility in our service area and feel you would benefit from an in-service to learn more about this, please call (860) 647-9798 x 249.
Physician’s Emergency Certificate (PEC): A PEC is required for the ambulance transport of a psychiatric patient going to any destination (typically a locked behavioral health unit) against their will (or by the will of the physician). In other words, they are being committed to the facility and their ability to make self determination is temporarily suspended by law.
A PEC must be an original form, typically demonstrated by being two-sided and often written in blue ink for this purpose. A copy cannot be used and it must be signed by a physician. It must accompany the patient and therefore cannot be faxed or emailed ahead as facilities will not accept a copy. This form is NOT used for voluntarily committed patients or patients who are conserved where the conservator has ordered transport.
This form also authorizes the ambulance crew to hold the patient against their will. In Connecticut, the only forms that allow an ambulance crew to hold a patient against their will are a PEC and an Emergency Examination Report issued by a licensed clinical social worker or a police officer. It is the policy of Aetna and ASM to also accept and enforce hospital and healthcare ‘Voluntary Commitals’ as granting authority to the ambulance crew to hold patients against their will. Ambulance crews must always use the minimum force necessary and most often this means simply confining the patient and does not necessarily mean the use of force or restraint.
Ambulance crews are not trained or equipped to subdue individuals. Chemical and physical restraints used by ambulance crews are intended to be applied with the assistance of law enforcement or healthcare staff. Judicious, prophylactic application of soft restraints should be strongly considered for patients that present a risk of elopement or danger to self and others. The back of an ambulance is not a controlled and static environment and this should be taken into consideration.
Transportation Authorization Certificate (TAC): A TAC compels the State of Connecticut to pay for the transportation of a patient in need of psychiatric care who is being admitted to an inpatient, state-operated facility. The receiving facility representative signs on Line 4 of this form and it is used as a check and balance before issuing payment to a transportation provider.
There are only five state-operated, inpatient psychiatric facilities in the state, Blue Hills, Cedarcrest (closed), Connecticut Valley Hospital (CVH), Greater Bridgeport Mental Health and Capitol Region Mental Health Center. An ambulance crew does NOT need this form if the destination is any other facility. The need for this form is not created by any other factor such as the chief complaint, the payor or the sending location.
W-10 (demographic portion of the discharge summary): Hospitals and skilled nursing facilities (SNFs) are required to provide the ambulance provider with enough information to safely complete the ambulance transport. Aetna and ASM are Covered Entities under HIPAA, have approved policies and procedures in this regard and all employees have been trained in appropriately handling protected health information (PHI). A hospital or SNF can restrict the amount of information they issue as long as the transport can be safely completed and sufficient information has been provided to carry out treatment, payment and healthcare operations.
Hospitals and SNFs are no longer required to provide a State of Connecticut W-10 form or a full discharge summary and quite often they send the summary electronically to the SNF. Although the W-10 format is not mandated, hospitals and SNFs must provide demographics, history, meds, allergies and any other pertinent information even if the patient is returning to a private residence without scheduled services.
No other form is required for routine BLS ambulance transport. Ambulance crews should NOT be looking for a full discharge summary, so-called “No Harm” letters, full medication administration logs (MARS), psychiatric notes, or any other form that is not listed above. EMTALA-type forms may be useful in informing an ambulance crew as to the patient’s condition and though they may be required paperwork, they are not for the ambulance crew.
Questions? Call the billing office at (860) 647-9798.
 I began my career in the Westport, CT, Fire Department in 2007 as a 20-year-old kid who had just achieved his lifelong goal of becoming a firefighter. During the first few years of my career, I became a volunteer with Donate Life CT to raise awareness about organ and tissue donation.
I began my career in the Westport, CT, Fire Department in 2007 as a 20-year-old kid who had just achieved his lifelong goal of becoming a firefighter. During the first few years of my career, I became a volunteer with Donate Life CT to raise awareness about organ and tissue donation.



 MANCHESTER and HARTFORD — The specialty bariatric stretchers operated by Aetna and ASM have now been equipped with
MANCHESTER and HARTFORD — The specialty bariatric stretchers operated by Aetna and ASM have now been equipped with  According to the Stryker website
According to the Stryker website Essential Performance Results
Essential Performance Results by Sam Porcello
by Sam Porcello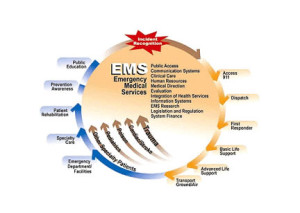 HARTFORD — On August 17, 2013 the Department of Public Health’s Office of Emergency Medical Services (OEMS) released a report entitled “A Reassessment of Emergency Medical Services” that represents a review of recommendations made by the National Highway Transportation Safety Administration’s Technical Assistance Team. The last such review was ten years ago.
HARTFORD — On August 17, 2013 the Department of Public Health’s Office of Emergency Medical Services (OEMS) released a report entitled “A Reassessment of Emergency Medical Services” that represents a review of recommendations made by the National Highway Transportation Safety Administration’s Technical Assistance Team. The last such review was ten years ago.

 GREG BORDONARO
GREG BORDONARO MANCHESTER — A free Continuing Medical Education course will be held Tuesday, July 23rd at the Ambulance Service of Manchester, 275 New State Road from 7:00 pm to 9:00 pm.
MANCHESTER — A free Continuing Medical Education course will be held Tuesday, July 23rd at the Ambulance Service of Manchester, 275 New State Road from 7:00 pm to 9:00 pm.